Eosinophilic Esophagitis (EoE) is a medical condition that has become increasingly recognized over the past two decades, but can still be challenging to get diagnosed. Find out more about it in our special EoE section that features two articles, one by three Canadian paediatric gastroenterologists for an overview on the condition and one featuring patient stories, sharing what it’s like to live with this condition as an adult and as a child.
Overview of EoE – featuring Canadian paediatric gastroenterologists
Tell me about Eosinophilic Esophagitis (EoE)
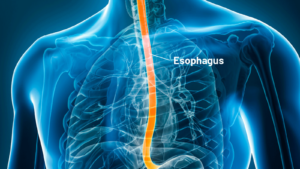
Eosinophilic Esophagitis (“ee-o-sin-o-fil-ik” “uh-sof-uh-jie-tis”), widely called EoE for simplicity, is a chronic allergic condition in which there are too many eosinophils (a type of white blood cell) in the esophagus. This leads to inflammation and may come with unpleasant symptoms.
Simply, EoE can be described as a condition with allergic inflammation of the esophagus. It may develop as a delayed allergic response to certain foods; EoE is considered a non-IgE-mediated food allergy and symptoms are generally not life-threatening and represent a slow build-up of eosinophilic inflammation. This is in contrast to IgE-mediated food allergy, which can potentially trigger a life-threatening allergic reaction (anaphylaxis). In some patients, environmental allergens may have a role in triggering the EoE.
EoE is increasing in frequency in Canada likely due to both a true increase and improved awareness. Symptom onset can be from infancy to older age.
Symptoms

Classic EoE symptoms often involve dysphagia, which is difficulty with eating and swallowing solid food. Patients say it feels like food is sticking in their chest or throat after swallowing. The foods which are most challenging to swallow (but not necessarily causing the EoE) include dry foods such as steak, chicken breast, rice and bread. Patients may have chest pain and/or heartburn along with difficulty swallowing.
Patients typically try to “wash” the bites of food down with water, avoid eating dry foods (or add a lot of sauces to help lubricate), take small bites often with water, and chew the solid food excessively, often making them slow eaters.
For children, in addition to difficulty swallowing, symptoms can include vomiting, having difficulty progressing from more smooth foods to solid foods, abdominal pain and even food refusal leading to poor growth.
Risk Factors
Certain patterns put individuals at higher risk of having EoE and help predict the likelihood of making a diagnosis. For simplicity, we can use a rule of about 2/3. Approximately 2/3 of patients are male; and approximately 2/3 have an allergic background which includes a history of asthma, eczema, environmental allergies and/or IgE-based food allergies. Having an immediate family member with known EoE or dysphagia certainly increases the risk but is not present in the majority of patients.
Diagnosis
It may take several years to get a diagnosis, as symptoms tend to be gradual, and patients adapt to them. The exception is if food is actually stuck and the patient cannot swallow their own saliva – this is called a food bolus impaction and requires urgent attention.
An endoscopy with biopsies (tissue samples) from the esophagus is required to make a diagnosis of EoE. This means a referral needs to be made to a specialist, typically a gastroenterologist, who can perform an endoscopy. An endoscopy involves placing a tube with a light and tiny camera down the throat to examine the esophagus. Biopsies taken during endoscopy will show an increased number of eosinophils in the sample of the esophagus; when diagnosing EoE there are more than 15 eosinophils per high power field when looked at under a microscope by a trained professional.
Treatment
EoE is a chronic condition and requires ongoing treatment. Treatment goals include improving symptoms, reducing inflammation, and preventing scar tissue and narrowing, medically termed fibrosis and strictures, respectively.
Treatment options each have their pros and cons. Issues such as ease, cost, sustainability, quality of life, possible adverse events, and effectiveness are some of the major factors that need to be balanced and discussed with your EoE specialist when collectively deciding on treatment.
In general, there are four treatment options to control esophageal inflammation.
- Proton Pump Inhibitor (PPI) – prescription antacid medication. This medication is most often used for treating reflux but has been demonstrated to help EoE patients and decrease eosinophilic inflammation in a way that is beyond acid suppression.
- Dietary elimination – “empiric” elimination diets remove foods which have been shown to trigger EoE in many patients, however identifying trigger foods for an individual patient remains challenging. Given that dairy (the milk protein, not the sugar, lactose) is one of the most common foods to trigger EoE, your doctor may start with a trial of eliminating dairy. If this is unsuccessful, your doctor may consider eliminating more foods from the diet. Patients should have the input of a dietitian familiar with EoE if undertaking a dietary elimination trial, so that nutrient deficiencies do not occur. Note, food allergy tests (skin tests and blood tests) are not helpful when trying to identify the foods that are triggering the inflammation in the esophagus.
- Swallowed topical corticosteroids – swallowing a local steroid which coats the esophagus has been shown to decrease inflammation. Numerous forms are available including a dissolvable budenoside pill, spray from an inhaler (puffer) directed to the esophagus (swallowed rather than inhaled), and a liquid slurry. The medication can be taken once or twice a day.
- Biologics – dupilumab is an injection therapy (under the skin) which has been more recently approved for the treatment of EoE, and other conditions such as severe eczema and asthma. It works by blocking the immune system’s recruitment signaling pathway and results in decreased inflammation. This product is presently not widely accessible due to high cost and is generally suggested when other treatments have not been tolerated, effective and/or the patient has several co-existing conditions (i.e., eczema, asthma) which require treatment.
Note: All treatments should be followed up with a repeat endoscopy and biopsies after adequate treatment duration to evaluate effectiveness for that individual patient as symptoms do not always match disease activity.
Take home points
- EoE is a condition that is being increasingly recognized in both adults and children.
- For most patients, it is a result of one or more triggering foods, but for some, environmental allergies may also play a role. Many patients will also have other allergic conditions such as asthma and eczema.
- Symptoms relate to allergic inflammation in the esophagus and often vary with age. Classic symptoms include difficulty swallowing foods, which may even get stuck in the esophagus, but other symptoms include heartburn, stomach pain, vomiting, and in young children, there may be some food refusal behaviours.
- It is diagnosed by finding increased eosinophils in biopsies (tissue samples) from the esophagus which are obtained during an upper endoscopy.
- Different treatment options exist and could include medical therapy and/or food elimination diets. Elimination diets should be done under the guidance of a registered dietitian. The choice of treatment should be a collaborative decision between the treating physician and the patient. The condition requires long-term monitoring.
Thank you to Dr. Vishal Avinashi, Dr. Mary Sherlock, and Dr. Jennifer Griffin, paediatric gastroenterologists who are part of the Canadian Pediatric EoE Network, for their expertise and support with this article on EoE!
Learn more
Download our 1-page sheet for a quick overview for yourself or to share with others.
 Webinars
WebinarsWatch our webinars: one for EoE in adults and the other in kids
Living with EoE
EoE affects both adults and kids. Read below to find out more about how members of our community are navigating this condition.
Nisha and Shayna: Adults with EoE
Can you tell us how your journey with EoE began? What signs and symptoms were you experiencing?

Nisha: I’ve had trouble swallowing since I was around 10 years old. Family and doctors often told me it was “all in my head” and that I just needed to eat more slowly. It was hard to describe what I was going through, especially as a child, so I believed them. Over time, my swallowing difficulties went from occurring weekly, to daily, to eventually with almost every meal.
Shayna: I have had EoE symptoms ever since I was little. I have always been the last to finish a meal and was known as a slow eater. While I knew there was something not right, I did not have the words to describe what it was.
When were you diagnosed, and what was your experience leading up to your diagnosis? Did you know anything about EoE beforehand?

Nisha: I didn’t seek medical help until one day when my dinner got stuck in my esophagus for hours. I couldn’t handle the pain and I went to the emergency department. I ended up having an endoscopy, they noticed the stricture and high eosinophil count, and I was diagnosed with EoE at 27 years old.
Before my diagnosis, I had never heard of EoE. Had I known what to look out for, I probably would’ve been more proactive in seeking appropriate medical attention well before the incident that led me to the emergency department. In any case, I had to go through a lot of testing to rule out other conditions like gastroesophageal reflux disease (GERD) and Crohn’s disease. The journey to a diagnosis was lonely, frustrating, and confusing – but I knew I had to keep pushing forward to get the right treatment for my condition.
Shayna: I was diagnosed in 2019 at the age of 23 after a long journey of many medical appointments and tests. I had seen an endocrinologist and internal medicine doctors without reaching a diagnosis. It was not until I saw a new allergist for a routine appointment where she asked the right questions, as she was very familiar with EoE. Other providers had asked if I got food stuck in my throat or if I had trouble swallowing, but my response was “no” because of the adaptations I’d been unconsciously making to eat.
For me, the brain-gut connection was also a big part of my symptoms. I experienced brain fog, fatigue, difficulty concentrating and exaggerated emotions between meals that was worsened by stress. Yoga helped with this before the diagnosis, but ultimately EoE management was the most impactful.
I did not know anything about EoE before and was so relieved to have found a diagnosis after so many evaluations coming back normal.
What is it like living with EoE, and how are you managing it?
Nisha: After my initial diagnosis, I was prescribed several medications, and my overall mood was quite low. While I felt liberated and relieved to have a firm diagnosis, it was overwhelming to learn that I had this condition I knew nothing about.
After experimenting with an elimination diet, we discovered that dairy was triggering my EoE. Over the years, I have managed to adjust my lifestyle to suit my needs and my EoE is improving. I’m also managing multiple food allergies.
Shayna: Luckily, taking medications, including a protein pump inhibitor (PPI) and a corticosteroid, has been a great treatment plan for me. I have eliminated dairy from my diet as well. I chose not to do the 2-4-6 elimination diet as I am allergic to peanuts, nuts, and sesame seeds, and I have celiac disease.
What would you like others to know about EoE?
Nisha: EoE can be overwhelming and take an emotional toll. As you go through your journey and educate yourself on EoE, share your knowledge with others. Your support system will appreciate this and help you navigate it as well. I found online communities where others shared their own experiences with EoE very helpful in alleviating feelings of loneliness and frustration. Stay strong!
Shayna: EoE is a hard diagnosis to finally find and it’s a journey to recovery. I will say after the esophageal tissue heals you will notice a dramatic improvement in quality of life and know what symptoms indicate a flare up. More education is needed for medical practitioners to ask the right questions for a quicker diagnosis.
Also, I want people to know that you are not a burden for having special dietary needs. I know it is hard to explain your allergens when meeting new friends/colleagues and going on dates, but trust me, there are some really good people who will understand and make accommodating look effortless.
Sebastian: Youth with EoE
Karin, how did your son Sebastian’s journey begin and what signs/symptoms was he experiencing?

Our son Sebastian has multiple food allergies, eczema, and asthma. Early on, he was on the petite side, and we were having frequent visits to the allergy clinic and paediatrician to monitor his growth. His main symptoms were poor weight gain and a very small appetite.
When he was 5 years old, he started telling us about the “bad tasting hot liquid that always comes up” and how he has to clear his throat or cough it back down. Then, my husband pointed out that our son was often coughing when eating, although just a little cough. I remember going to my son’s allergy appointment a few weeks later and mentioning the “bad tasting hot liquid” and his “asthma” cough being more prevalent when eating food.
When was he diagnosed, and what was your experience leading up to his diagnosis? As a parent, did you know anything about EoE beforehand?
After the allergy appointment, we met with a gastroenterologist, then eventually our son had an endoscopy which confirmed EoE. On this journey, our son had so many doctor’s appointments and was pretty over the entire process and was not willing to be examined any more. There were a few major hospital meltdowns leading up to the endoscopies.
I had heard about EoE in my allergy parent Facebook groups and the only thing I knew was that it was something we didn’t want.
What has it been like living with EoE, and how is he managing it?
Nobody knows what it is and it’s really difficult to explain to people. In our son’s case, his team of doctors—gastroenterologist, allergist, dietitian—advised that further food restriction was not advisable with how many foods he is allergic to. In the end, the treatment that has worked best for him is a daily mix of medications, and he is very responsible with taking them.
It was really amazing to see the complete turnaround with his hunger, eating, and mood once he started treatment. It was like a calm suddenly came over him and it made us realize that he must have been really uncomfortable for a long time.
We feel grateful that the doctors didn’t brush aside our son’s symptoms, he was able to start treatment so early on, and he has had such a wonderful team looking out for him.
What would you like others to know about EoE?
For others facing an EoE diagnosis, there is treatment and improved quality of life afterwards. EoE can be managed. Our son would like people to know that it is hard but there are worse diseases. He doesn’t really have to think about EoE now that he takes medication. Sebastian is really into soccer and plays 4 days a week, EoE hasn’t slowed him down!
Thanks Nisha, Shayna, Karin and Sebastian for sharing your experiences with EoE and helping to spread awareness of this condition!
Learn more
Download our 1-page sheet for a quick overview for yourself or to share with others.
 Webinars
WebinarsWatch our webinars: one for EoE in adults and the other in kids