Check out our advocacy in action around labelling on self-care products and “May contain” statements. If you’re a university student, find out how you can participate in research to better understand how food allergies are supported on campus. Plus read about the latest in research, including how eating fatty fish can reduce asthma symptoms in children, how anaphylaxis occurs so quickly, and how common adult-onset allergy is. You can also bust our latest myth!
Advocacy in action: Update on self-care product labelling in Canada
 In 2016, Health Canada had an open consultation on improving regulations on self-care products (e.g. vitamins, supplements, cosmetics, shampoo, etc.). Many of you also responded to our call to action at that time to let Health Canada know that self-care products should have labelling requirements and list priority allergens like pre-packaged food products.
In 2016, Health Canada had an open consultation on improving regulations on self-care products (e.g. vitamins, supplements, cosmetics, shampoo, etc.). Many of you also responded to our call to action at that time to let Health Canada know that self-care products should have labelling requirements and list priority allergens like pre-packaged food products.
Last month, we presented our recommendations as part of Health Canada’s technical briefing with key stakeholders, including Health Canada, CFIA, industry, and other patient organizations. We re-iterated our recommendations for improved allergen labelling and the need to have ingredient information in order to make informed decisions when purchasing self-care products.
These recommendations will be put forward by Health Canada as they move to finalize the updated regulations in early 2019:
- Require manufacturers to provide a complete and accurate ingredient list that includes priority food allergens for each product
- Use plain, simple language for priority food allergens, as currently required for pre-packaged food products, e.g. whey (milk)
- Follow similar labelling requirements as regulated by Health Canada for pre-packaged products that require priority allergens to be declared in the list of ingredients, OR in a “Contains” statement
- Follow Health Canada recommendations if manufacturers elect to use precautionary statements for priority food allergens. Health Canada has recommended the single statement “May contain” when precautionary labelling is needed.
By making these changes to the regulatory framework, you and all Canadians with food allergies will have access to key ingredient information when selecting self-care products so you can better manage your food allergy and avoid having allergic reactions.
We will keep you posted on this important initiative. Thanks again for you support in creating change!
Advocating around the world: Calling for action on precautionary allergen labelling
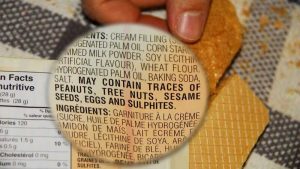 Last month, we led an initiative with 21 other patient organizations from around the world to submit a letter to the Codex Alimentarius Commission on the issue of precautionary allergen labelling (e.g., “May contain” statements).
Last month, we led an initiative with 21 other patient organizations from around the world to submit a letter to the Codex Alimentarius Commission on the issue of precautionary allergen labelling (e.g., “May contain” statements).
The Codex Alimentarius Commission develops internationally recognized standards, codes of practice, guidelines, and other recommendations relating to foods, food production, and food safety.
Currently there are no consistent or standard methodologies for using precautionary allergen labelling globally, which poses safety concerns for individuals with food allergies. The letter to Codex calls for them to address this issue using a scientific risk-based approach, which will then allow consumers to make safer, more informed food choices and provide food manufacturers with greater clarity when making allergen labelling decisions.
As a part of this global patient coalition, we are committed to advocating on your behalf on this issue. We will keep you updated on the progress we make.
Research: University students – participate in a new study
 If you are a university student with food allergies attending McGill University, McMaster University, Queen’s University or the University of British Columbia, you are invited to participate in a research study looking at the experiences of university students with food allergies.
If you are a university student with food allergies attending McGill University, McMaster University, Queen’s University or the University of British Columbia, you are invited to participate in a research study looking at the experiences of university students with food allergies.
How to participate
Please complete a short, online survey. It should take up to 10 minutes to complete.
- Survey link: www.surveymonkey.com/r/foodallergystudentsurvey
- The survey closes on February 28, 2019
Survey details
Survey findings will help researchers, and patient organizations like ours, better understand how students with food allergies are supported on campuses. All data collected will remain anonymous.
If you have any general questions about the study, please contact Ernie Avilla, Research Coordinator, McMaster University, Canada at avillae@mcmaster.ca or call 289-921-8716.
Share, share, and share! Please spread the word and share the survey with students attending these institutions.

Research: Eating fatty fish can reduce asthma symptoms in children
An international study has found that children with asthma who followed a healthy Mediterranean diet enriched in fatty fish (like salmon, trout, and sardines), had improved lung function after six months.
Research: Researchers use mice to identify how anaphylaxis occurs so rapidly
 Researchers at Duke Health, published a study in the journal Science, used mouse models to track how immune cells are triggered during anaphylaxis. They describe a previously unknown mechanism in which a newly identified immune cell basically mines the blood vessels for allergens and then utilizes an unusual mechanism for rapidly delivering the blood-borne allergens to mast cells.
Researchers at Duke Health, published a study in the journal Science, used mouse models to track how immune cells are triggered during anaphylaxis. They describe a previously unknown mechanism in which a newly identified immune cell basically mines the blood vessels for allergens and then utilizes an unusual mechanism for rapidly delivering the blood-borne allergens to mast cells.
The finding potentially opens up innovative ways to shut down anaphylaxis from happening.
Research: Adult-onset food allergy is fairly common
 One in four surveyed adults with food allergies reported developing their allergy after childhood, with women more likely to report an adult-onset food allergy than men.
One in four surveyed adults with food allergies reported developing their allergy after childhood, with women more likely to report an adult-onset food allergy than men.
The survey was administered to 40,443 adults in the U.S. between 2015 and 2016. Self-reported food allergies were validated by symptoms consistent with IgE-mediated reactions. Shellfish allergy was the most common allergic reaction reported by adults (13.3%) with food allergies, followed by milk (6%), wheat (5.6%), tree nut (4.8%), and soy (3.9%).
Mythbuster: Someone who has been treated with an epinephrine auto-injector (e.g. EpiPen®, AUVI-Q®) doesn’t necessarily need to go to the hospital

FACT: Anaphylaxis is a life-threatening condition which is treated by a medication called epinephrine. Epinephrine is a short acting medication that can counteract some of the issues that arise including airway closure and decreased blood flow to the heart and brain. When someone is having a severe allergic reaction or anaphylaxis, epinephrine is used to help start treatment prior to going to the hospital.
There are also important “co-factors,” such as alcohol, exercise and certain medications, that can influence the severity of food allergic reactions by lowering the threshold for a reaction in some people.
Bottom line: Sometimes more help is needed than just using epinephrine, which is why it’s necessary to go to the hospital.
Help us educate your communities and share this Mythbuster with them! Stay tuned for more Mythbusters to come.
Medical content reviewed by: Dr. Zainab Abdurrahman, MD, MMath, FRCPC, and Dr. Julia Upton, MD, FRCP(C) Clinical Immunology and Allergy
Check out our blog for other myths about:
- Some allergies are more “severe” than others
- Eating a little allergen will increase tolerance and cure allergy
- Age requirement for allergy testing
- Cooking at high temperatures kills allergen proteins
- “May contain” allergen labelling is mandatory
- Results of skin prick tests indicate severity of allergy
- Pesticides and other chemicals can trigger allergies
- Epinephrine auto-injectors cure food allergy
- Which allergens cause life-threatening reactions
- Using Benadryl
- Food allergy “cures”
- Celiac disease is the same as a wheat allergy
